AML is the most common acute leukaemia in adults and incidence is on the rise, partly due to population ageing. Despite the emergence of new targeted therapies for AML patients, survival rates remain dismal (~27% at 5 years). Current challenges include the rapid development of resistance and the inability to predict which therapy is optimal for each patient, especially for those without ‘actionable’ mutations. These challenges are compounded by the lack of complete testing platforms for capturing critical patient-specific molecular profiles beyond somatic mutations, such as changes in the proteome and phosphoproteome. Due to the heterogeneous nature of AML, individualised screening and personalised treatment plans are likely required to improve treatment and survival outcomes for AML patients.
By combining genetic profiling, phosphoproteomic and proteomic analysis, we have developed a pipeline for profiling AML patient samples. Using this pipeline, we have identified novel therapies for different leukaemia subtypes ( Leukemia, 2021). In this study, we have integrated genomic, proteomic, and phosphoproteomic profiling together with ex vivo drug sensitivity profiling for a functional read-out of drug sensitivity or resistance, to identify optimal therapeutic regimes for individual AML patients.
Ex vivo drug sensitivity profiling has been performed on 71 patients. Genomic profiling was performed using the SOPHiA Genetics Myeloid Panel. The mutation frequency identified was similar to previous reports ( TCGA, N Engl J Med 2013). The drug screen panel included AML standard of care treatments (e.g., cytarabine, midostaurin) as well as investigational agents. Cell survival was measured at 24 hours using an ATPlite assay or Annexin V staining. Results identified both known and novel associations with mutation subgroups. Consistent with previous reports ( Jawhar, Blood 2017), IDH2 mutations were associated with reduced sensitivity to midostaurin (p=0.0039). Samples with NPM1 mutation were significantly more sensitive to Aurora kinase/CDK inhibitor JNJ7706621 compared to NPM1 wildtype (p=0.0007). This association also held true in the BeatAML cohort (Vizome, p<0.0001). NPM1 has documented roles in cell cycle regulation, and these results suggest that mutant NPM1 may sensitise to cell cycle targeted therapies. Multi-omic analyses of 23 intermediate/high risk patients, 9 of which had no actionable mutations, identified further drug vulnerabilities, with >2 therapies identified for each patient.
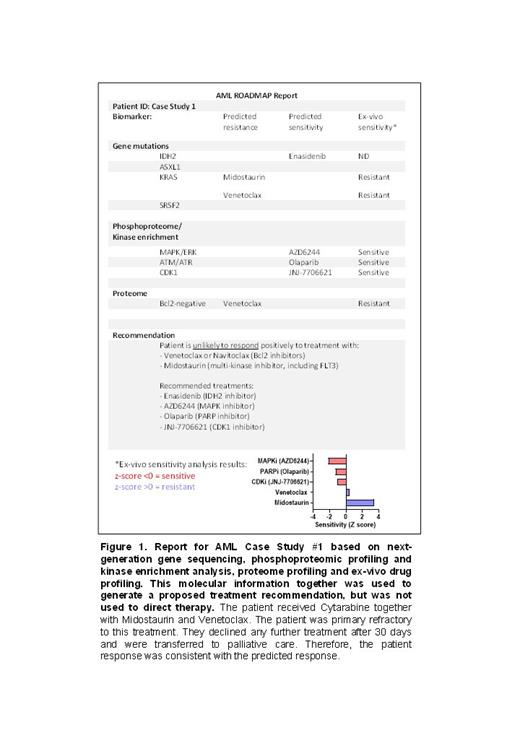
Validation of this approach is exemplified by individual case studies where our profiling platform correlates with clinical outcome. In the first case, the patient presented with a KRAS mutation, predictive of resistance to midostaurin. Proteomic profiling identified low expression of BCL2, predictive of resistance to venetoclax. Phosphoproteomic profiling however identified activation of DNA repair and CDK proteins, suggesting sensitivity to DNA repair and CDK inhibitors. Ex vivo drug sensitivity profiling of the patient blasts identified resistance to midostaurin and venetoclax, but sensitivity to PARP and CDK inhibitors. Concurrently, the patient received a combination of standard chemotherapy and targeted therapy (cytarabine, midostaurin, venetoclax) and was primary refractory to treatment.
In a second case, proteogenomics and ex vivo screening predicted sensitivity to midostaurin and venetoclax. The patient received cytarabine, midostaurin, and venetoclax therapy and achieved remission. In our third case study, ex vivo screening predicted sensitivity to standard of care agents (cytarabine, midostaurin, venetoclax). While the patient achieved remission with standard of care chemotherapy, they subsequently relapsed. At relapse, ex vivo screening identified reduced sensitivity to cytarabine but a high level of venetoclax sensitivity. The patient was placed on FLAG with venetoclax and was bridged to transplant.
Therefore, our approach can predict treatment sensitivities and resistance to standard of care therapies, and may also identify alternative clinically available therapies. The results of these and further case studies will be presented at the meeting.
Disclosures
Enjeti:AbbVie: Honoraria, Speakers Bureau; Astellas: Honoraria; RACE oncology: Honoraria; Jazz: Honoraria; Pfizer: Honoraria; Otsuka: Honoraria, Speakers Bureau; Servier: Honoraria. Verrills:Race Oncology: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal